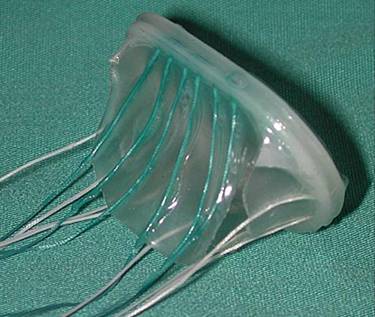
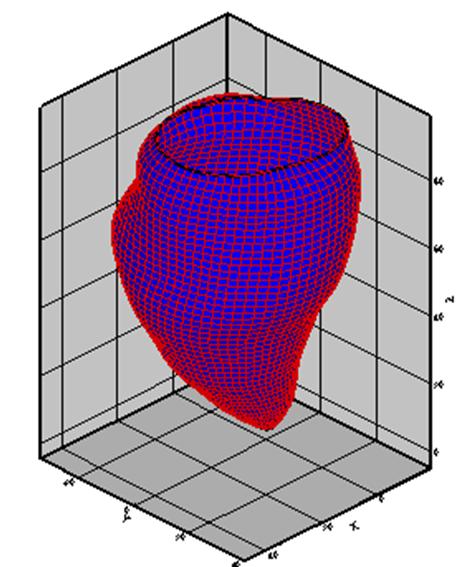
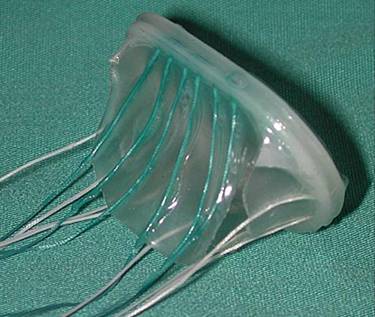
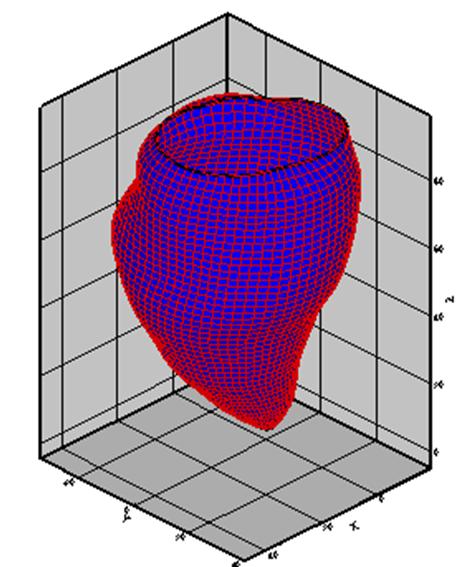
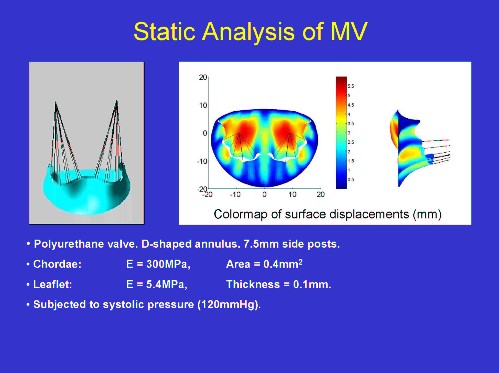
A bioprostheic MV design(left), the fibre mesh of MV (middle), and a prescribed dynamic LV model (right)
In human, the mitral valve is a complex anatomical structure consisting of two leaflets, an annulus, chordae tendineae, and papillary muscles. Different to the aortic valve, the leaflets of mitral are asymmetric, and are attached to the left ventricle through a bundle of chordae tendineae, which have a significant effect on its function. A diseased mitral valve is usually repaired by various surgical means such as to replace or transfer the damaged chordae. When a mitral valve is too severely diseased for repair technique to be effective, it is generally replaced with a mechanical or bioprosthetic valve. Understanding native mitral valve dynamic behaviour is thus highly important for developing more efficient repair techniques, and perhaps even more so for designs of artificial mitral valves. With improved cardiopulmonary bypass, myocardial protection, and surgical techniques, the mortality rate from aortic valve replacement decreased substantially, whereas the mortality rate from mitral valve replacement remains high (around 50% at 10 years), largely because of the low cardiac output syndrome.
To handle the dynamic modelling, we use the immersed boundary method, modelling the 3D dynamic fluid-structure interactions. The immersed boundary method is a practical and effective way to simulate certain types of fluid-structure interaction (FSI) problems (Peskin, 1989), which uses the elastic fibres to represent the elastic body (heart valve) immersed in a viscous incompressible fluid (blood). Its effective dynamic capability has been used to model blood flow patterns in the heart, and to assist prosthetic valve design.
To investigate the mechanical behaviour of the mitral design under physiological flow conditions without having to model the left ventricle, we make use of in vivo magnetic resonance images of the left ventricle. The relative motion of the mitral annulus and the papillary muscle regions of the ventricle determined from these MRI images is then used as a prescribed boundary condition for the chorded mitral valve in a dynamic cycle. Results show that without the proper functioning of the papillary muscle, the mitral prosthesis can suffer from an intolerable over-stretch during systole compared with laboratory tests in which the mitral chordae are fixed in space. This turns out to be the key weakness of the current design.
Current work involves modelling of human MV using a finite element IB method, with structure-based constitutive laws.
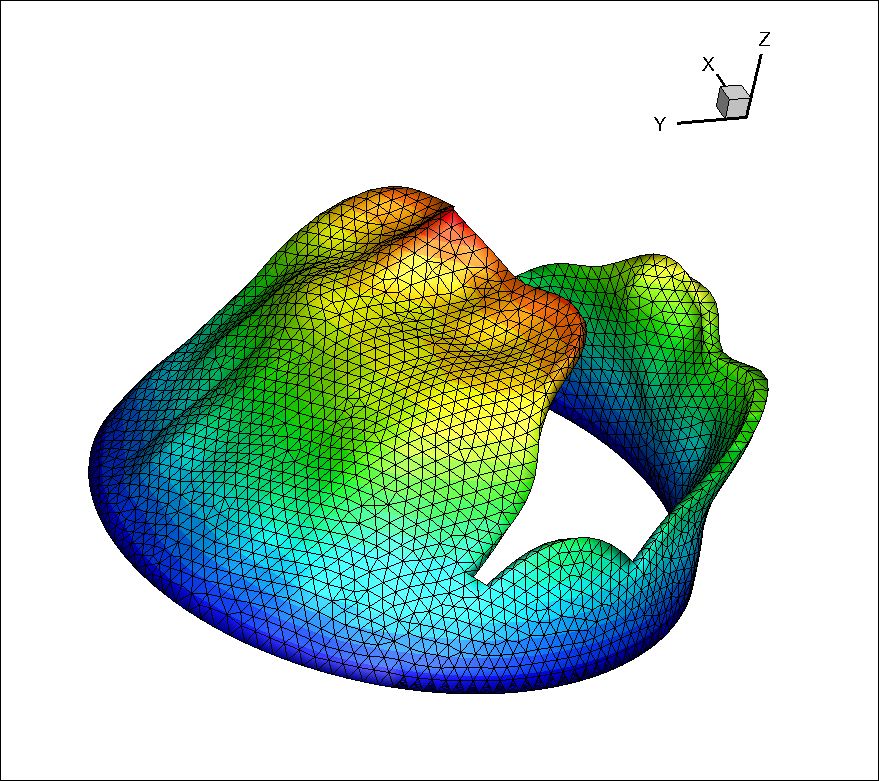
A human MV generated from MRI.
This work is in collaboration with
For more animations, see our group website.
Move up to Prof. X. Y. Luo